AMR in Malaysia
Introduction
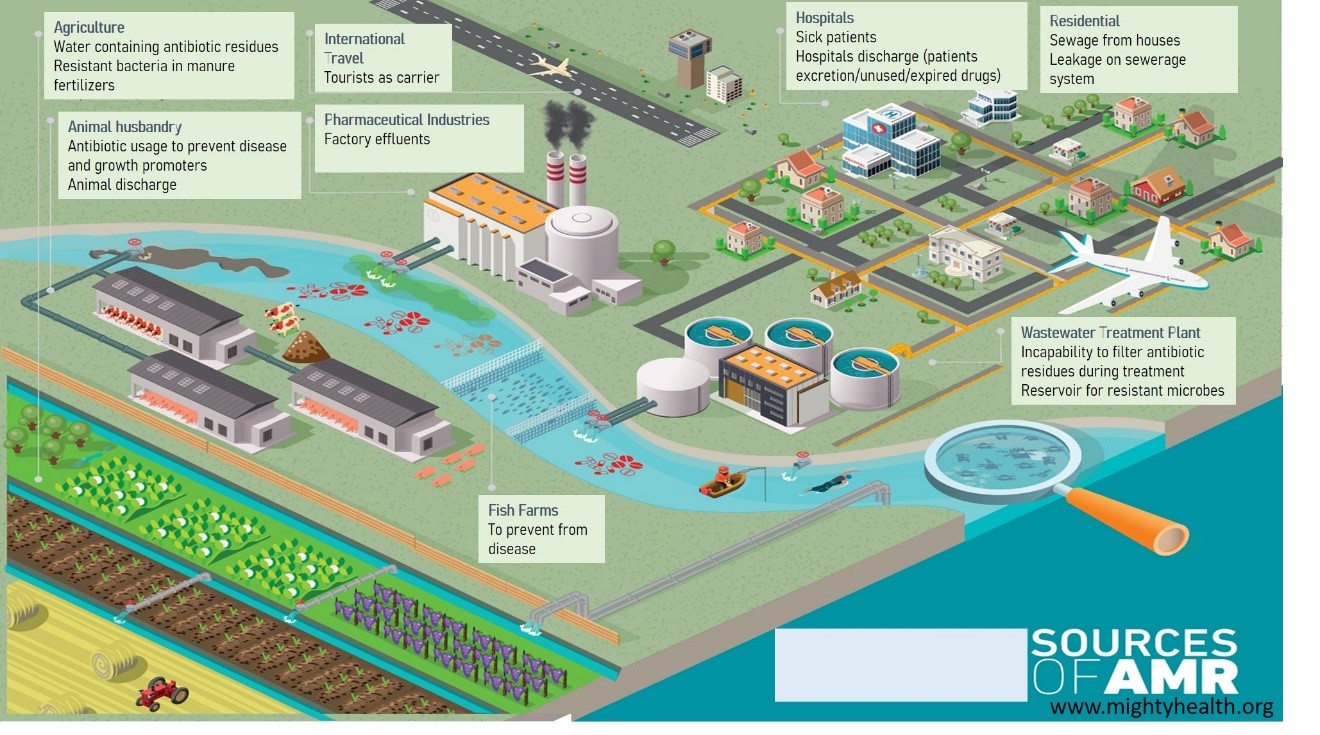
Many of the hurdles to combating antibiotic-resistant infections in the human health, animal health and food chain are well understood. However, the emergence of AMR in environment sector (water bodies) is a complex and multi related to various factors. Water is one of the key vectors for the emergence of antibiotic pollution, pathogens and resistance genes.
Human excreta and wastewater are recognized and documented as major sources of antimicrobial agents, their metabolites, antimicrobial-resistant bacteria and their AMR genes due to overuse of antimicrobial agents. Not to mention effluents from households, hospitals and pharmaceutical facilities, agricultural run-off, combined with direct contact between natural bacterial communities and discharged resistant bacteria, is driving bacterial evolution and the emergence of more resistant strains. If the concentrations are high enough, this can trigger resistance genes. Once this has happened, the risk of transfer to other places and to pathogens becomes just a matter of time.
There is growing public health concern that antimicrobial-resistant bacteria and AMR genes that enters our water sources via untreated or treated wastewater effluent and its exposure to us that use such water as drinking-water sources, for bathing, washing, primary contact recreation and as irrigation water.
Responsible manufacturing, usage and management of antibiotics must go hand in hand with waste and effluent management.
Facts
- Human antibiotics use up 36% this century; antibiotic use in livestock to grow 67% by 2030.
- Up to 75% of antibiotics used in aquaculture may be lost into the surrounding environment.
- Antimicrobial resistance is one of six emerging areas of concern highlight in UN Environment Frontiers Report 2017
- Antibiotic has been included in European Commission Surface water Watch List (WL) as a potential water pollutants that should be carefully monitored and determine the risk they pose to the aquatic environment. These include several macrolides (erythromycin, clarithromycin and azithromycin), amoxicillin and ciprofloxacin.
- One of the five strategic objectives in the WHO Global Action Plan is to reduce the incidence of infection through effective water, sanitation (WASH) facilities.
ANTIBIOTICS POLLUTION CONTRIBUTORS IN THE ENVIRONMENT:
- Agriculture: usage of manure fertilizers containing AMR
- Animal Husbandry: Antibiotic usage to prevent disease and growth promoters; animal discharge containing AMR
- Pharmaceutical industries: untreated factory effluent discharge to water bodies
- Tourism: Human as healthy AMR carrier
- Hospitals: hospital effluent discharge, expired drugs
- Residential areas: sewerage, leakage sewerage system may contaminated groundwater supplies
- Wastewater treatment Plants: incapability to treat antibiotic residues; reservoir for multidrug resistant microbes
HOW TO CONTROL AMR SPREAD IN ENVIRONMENT:
Public people:
- Do not flush/ throw expired/unused antibiotics in drainage system. This will lead to accumulated antibiotic residues in wastewater treatment plant and water bodies.
- By practicing good hygiene to reduce the risk of getting infectious disease.
Policy makers:
- Advocate for regulation of release of antibiotics from manufacturing facilities
- Improved handling/treatment of waste from sewage treatment plants.
- investments in high quality WASH infrastructure